Mary-Claire King is Professor of Genome Sciences and of Medicine (Medical Genetics) at the University of Washington (Seattle, WA), who first described a single gene on chromosome 17q21 (which she named BRCA1) being responsible for breast and ovarian cancer in many families. This work, published in Science in 1990, also revolutionized the study of many other common, single-gene diseases that are inherited in nature, and led to the discovery of BRCA2.
She, along with Dr. Jean Louis Mandel (discoverer of the genetic abnormality responsible for Fragile X Syndrome), participated in a plenary discussion at the recent European Society for Human Genetics conference in Barcelona Spain May 21-24, 2016 entitled “My vision on Genomic Medicine”. By way of background, BRCA1 and BRCA2 mutations account for 20-25 percent of hereditary breast cancers and 5-10 percent of all breast cancers. In addition, these mutations account for about 15 percent of all ovarian cancers; according to the American Cancer Society, in 2014 in the United States, of 235,000 new cases of breast cancer, BRCA1/2 account for 12,000 to 23,000 new cases; and of 22,000 new cases of ovarian cancer BRCA1/2 account for another 3,300 new cases yearly.
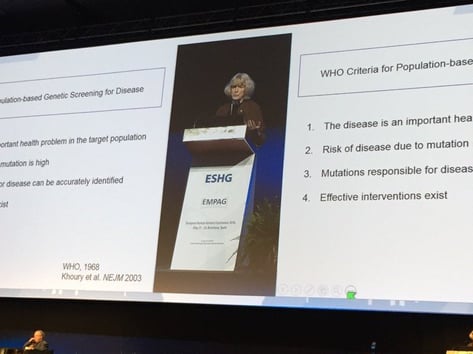
She began her comments by pointing to a 2003 New England Journal of Medicine (NEJM) paper with the title “Population screening in the age of genomic medicine” (note: the first author, Muin Khoury, is the founding director of the Center for Disease Control’s Office of Public Health Genomics). She described four criteria for public health screening: solving an important public health problem, the risk of disease is high, there is an ability to accurately identify mutations, and the presence of effective intervention. A 2014 study in Proceedings of the National Academy of Sciences (PNAS) showed the effectiveness of population-based screening and risk to BRCA1/2 carriers with or without family history of disease. With those with deleterious BRCA1 mutations, >80% will have cancer by age of 70; with BRCA2 mutations, the rate is >70%. This risk remains high even if there is no affected relative; this work is a powerful argument for screening to identify many carriers who are not evaluated due to lack of family history criteria.
She then referred to this 2002 NEJM paper http://www.ncbi.nlm.nih.gov/pubmed/12023992, describing that the risk of breast cancer is reduced but is not eliminated with surgery (salpingo-oophorectomy, the removal of the fallopian tubes and ovaries). The Kaplan-Meier curve from this paper (available online here: http://www.nejm.org/doi/full/10.1056/NEJMoa020119) demonstrates the dramatic reduction in the risk of death over time.
In many populations, there are recent, rare BRCA1/2 mutations which were not able to be discovered until the advent of next-generation sequencing.
Dr. King concluded her talk about the actionability of BRCA’s function and the use of poly ADP ribose polymerase (PARP) inhibitors for treatment. BRCA1and BRCA2 (also PALB2) are proteins important for the repair of double-stranded DNA breaks by homologous recombination repair (HRR). With mutated BRCA genes, the ‘backup’ mechanism for DNA repair is PARP1, and by inhibiting the function of PARP1, cancerous cells will not have their DNA with double-strand breaks efficiently repaired, leading to cell death. This novel approach for cancer treatment, called ‘synthetic lethality’, was significant for discovery of a new therapy with few side effects by leveraging current understanding of cancer biology. In late 2014, olparib was approved for treatment of cancer patients with germline BRCA1 or BRCA2 mutations, in breast, ovarian or prostate cancers.
Lastly Dr. King declared “No woman should die of cancer with a BRCA1/2 mutation”, and proposed that every woman be offered complete BRCA1/2 gene sequencing at the age of 30 as part of routine medical care; with individuals with severe family history, the sequencing of all related ovarian and breast cancer genes. (Dr. King has developed such a gene panel test called BROCA at the University of Washington; more information available here: http://web.labmed.washington.edu/tests/genetics/BROCA).
In the Question and Answer session following, the question was raised whether other screening (e.g. mammography) would be replaced by BRCA1/2 screening; Dr. King felt that stratification of frequency of mammography would occur based upon genetic status.
Another question centered around databases and their completeness. Dr. King sees the need for one for only physician use (where only ‘unquestionably pathogenic’ mutations are referenced) and a research use one. As a follow-up, since the private Myriad database of BRCA variants is not accessible (covering 20 years’ worth of BRCA testing with over one million samples analyzed), Dr. King noted that there isn’t any knowledge of the patient’s outcome after their genetic test results were returned.
Would you be interested in future developments for inherited disease reference materials? Sign up here to receive notification.




